Arthrofibrosis is a complex and often misunderstood condition that can occur after knee surgery, particularly after total knee replacement (TKR) , ACL reconstruction, or manipulation under anaesthesia (MUA). It involves excessive scar tissue formation, leading to stiffness, pain, and reduced range of movement (ROM). For many patients, this condition can be frustrating and debilitating limiting recovery and impacting quality of life.
This blog aims to explain what arthrofibrosis is, why it happens, and what can be done to support recovery, including the importance of early mobilisation, mechanical stretching, systemic inflammation, diet, and the evolving understanding of different subtypes of the condition.
What Is Arthrofibrosis?
Arthrofibrosis occurs when the body overproduces fibrous scar tissue in response to injury or surgery. While some scar formation is normal and part of healing, excessive or disorganised scar tissue can restrict joint movement and cause persistent pain.
This condition is not simply ‘post-operative stiffness’ it’s a pathological response that creates dense adhesions within the joint capsule, limiting the joint’s normal glide and flexibility. Symptoms may include:
- Loss of ROM (especially extension and flexion)
- Pain, particularly at end ranges of motion
- Persistent swelling or inflammation
- A feeling of tightness or ‘contraction’ in the joint
At a biological level, arthrofibrosis involves an overactive wound healing response. After surgery, fibroblasts (cells that produce collagen) and myofibroblasts (specialised cells that contract and remodel tissue) become activated. In arthrofibrosis, these cells remain active longer than necessary, laying down excessive collagen and causing contractures.
📘 Download Your Free Arthrofibrosis Tips Guide
Take your first step today. Download our free resource to help you structure your recovery at home.
⬇ Download NowWhy Does Arthrofibrosis Happen?
Several risk factors contribute:
- Surgical trauma – extent of dissection and bleeding
- Delayed mobilisation – lack of early movement can allow adhesions to form
- Genetic predisposition – some individuals naturally produce more scar tissue
- Chronic inflammation – perpetuates the fibroblastic activity

The Two Subtypes: Hot vs Cold Arthrofibrosis
Recent thinking has begun to differentiate between two presentations of arthrofibrosis:
1. Hot, Active (Pro-Inflammatory) Arthrofibrosis:
- Marked by ongoing inflammation
- Redness, warmth, swelling around the joint
- Patients may describe a “burning” or inflamed feeling
- Pain is often more significant, even at rest
2. Cold, Inactive (Chronic Scarred) Arthrofibrosis:
- Less swelling or redness
- Joint feels tight, restricted and fibrotic
- May occur after inflammation has settled but stiffness remains
- Responds more readily to mechanical stretch and scar remodelling
Identifying which type of arthrofibrosis a patient is experiencing can help guide treatment. For example, active inflammatory cases may need to focus more heavily on reducing inflammation and ensuring appropriate pain relief to enable high intensity mobilisation and stretching to commence.
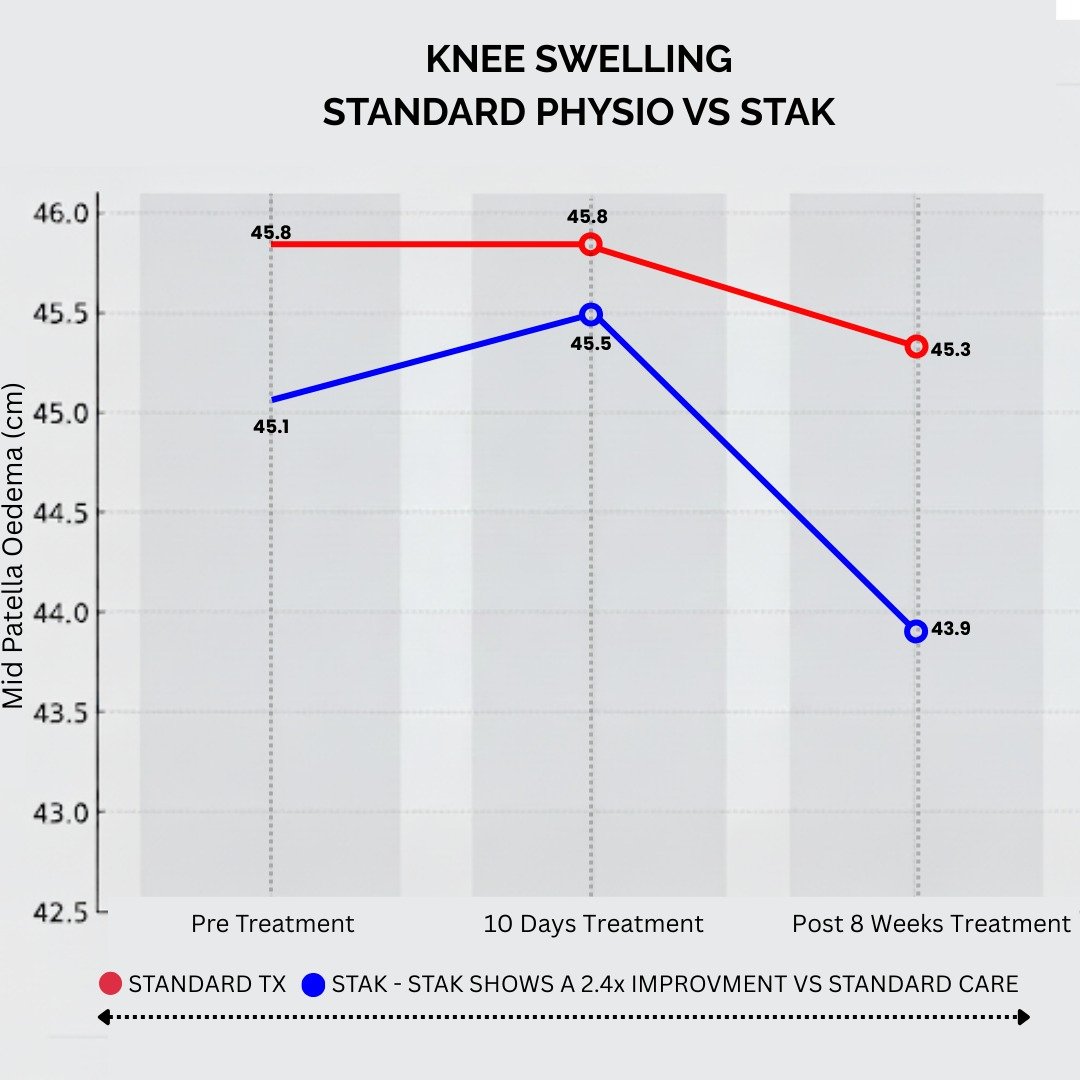
High-intensity stretching – such as with the STAK device – may do more than just break up scar tissue. We are finding early signs that it can actually reduce inflammation and swelling in the joint, too (see graph). This is an exciting observation, and it aligns with emerging research showing that vigorous exercise can induce anti-inflammatory effects in the body.
We plan to investigate this further, as it could mean intense stretching not only fights scar tissue but also calms the arthrofibrosis “fire” at its source. Follow our future blogs for more information on this topic!
The Role of Icing in Arthrofibrosis
Cold therapy (cryotherapy) can be useful in managing symptoms of arthrofibrosis especially the hot, inflamed type. It helps to:
- Reduce acute inflammation
- Decrease pain and swelling
- Improve tolerance to rehabilitation exercises
However, it’s important to use ice judiciously:
- Apply for 10-20 minutes at a time
- Protect skin with a cloth barrier
- Avoid icing immediately before stretching (as it may reduce tissue elasticity)
Some patients benefit from alternating heat and cold to improve circulation and reduce stiffness.
The Importance of Early Movement and Mechanical Stretch
Early, consistent movement is one of the most important strategies to reduce the risk of arthrofibrosis. Movement helps modulate collagen production and ensures scar tissue remains aligned and mobile rather than dense and restrictive.
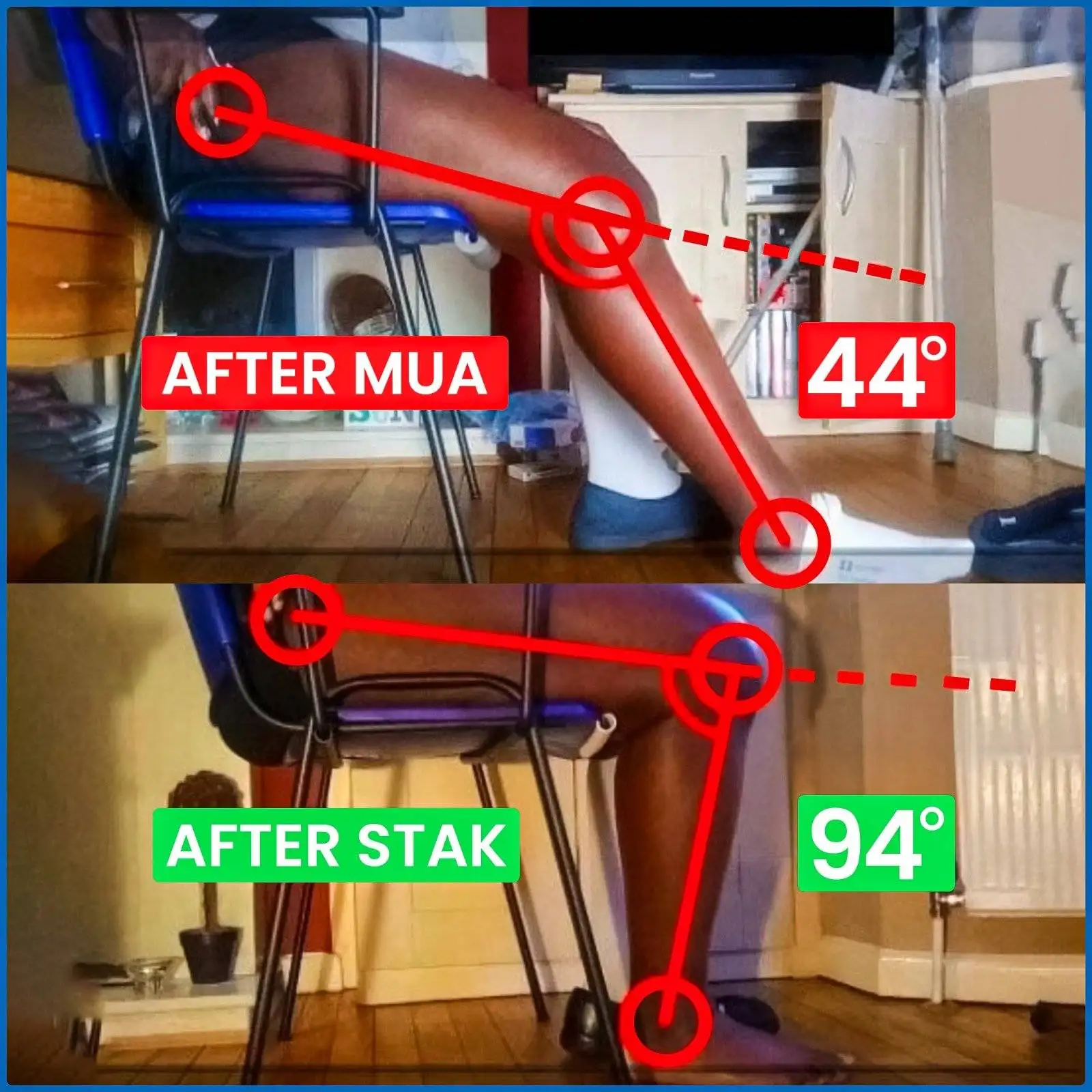
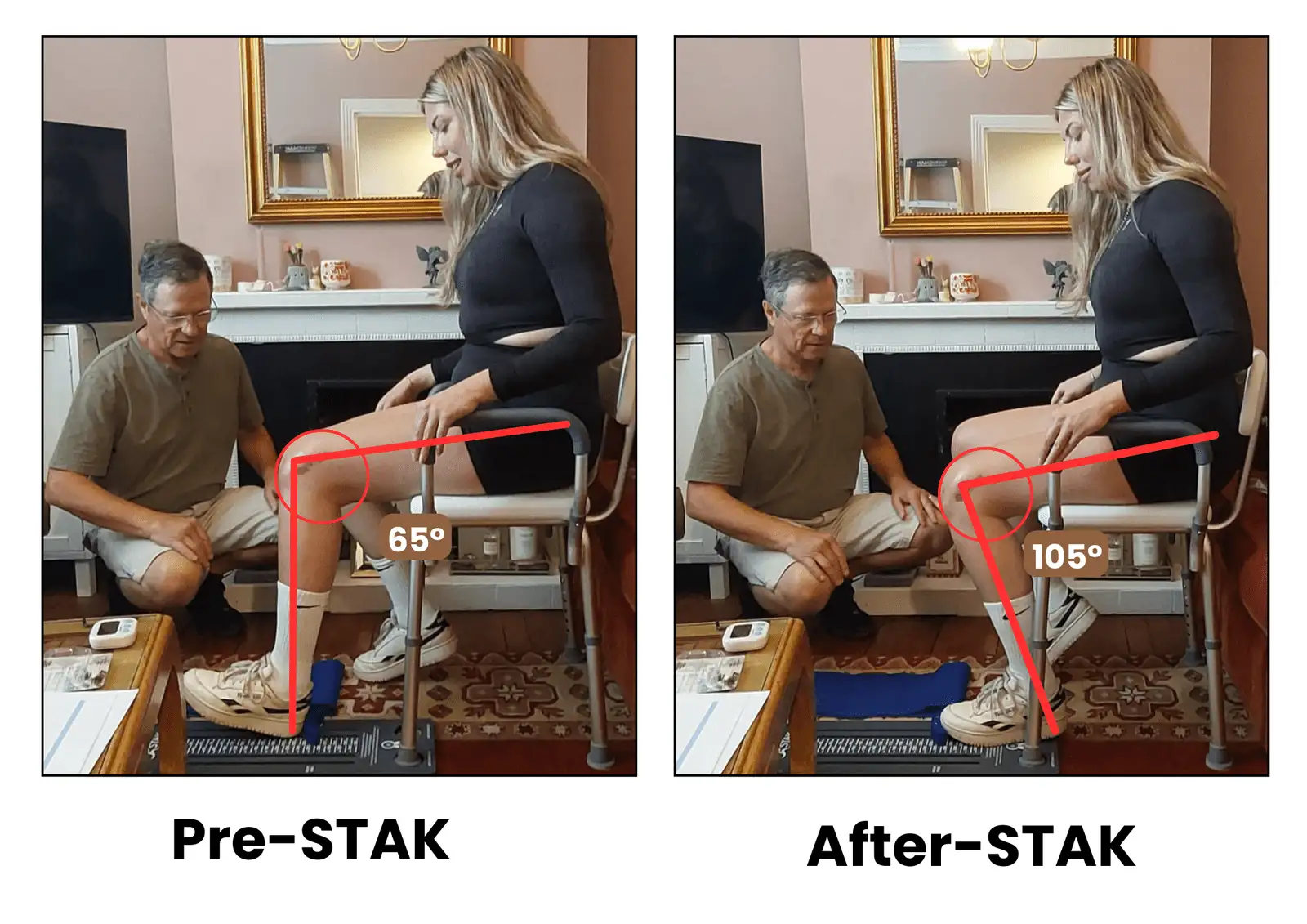
Devices like the STAK (Specialist Therapy Active Knee stretcher) are designed specifically for this purpose. STAK supports patients by:
- Allowing safe, progressive high intensity stretching and active stretching
- Enabling at-home control and consistency
- Encouraging patient engagement and confidence
Clinical trials and NHS implementation have shown that mechanical stretching can significantly improve ROM, reduce the need for further surgery, and support patient satisfaction.

Beyond Movement – The Role of Diet and Systemic Inflammation
Chronic systemic inflammation doesn’t just affect general health—it can contribute to an overactive scarring response. Supporting the body nutritionally may help optimise the healing environment.
Omega-3 Fatty Acids
- Found in oily fish (salmon, sardines), flaxseeds, walnuts
- Contain EPA and DHA, which reduce pro-inflammatory cytokines
- May reduce fibroblast overactivation and support healthy remodelling
Other Key Nutrients:
- Vitamin C – essential for collagen formation
- Zinc – supports tissue repair
- Magnesium – calms the nervous system and supports muscle relaxation
- Antioxidants – from berries, green tea, and colourful vegetables, help reduce oxidative stress
Hydration and avoiding processed sugars and seed oils also support an anti-inflammatory internal environment.
While diet alone won’t reverse arthrofibrosis, it forms an important part of a whole-body approach to healing.
Supporting Mental and Emotional Recovery
The emotional toll of prolonged recovery is often underestimated. Chronic pain, reduced mobility, and frustration with progress can affect mood, sleep, and confidence. Patients may feel isolated or disheartened.
Recovery is not just physical. Supportive physiotherapy, access to community, and understanding that healing takes time can dramatically improve outcomes. For many, partnering with a specialist who understands arthrofibrosis can make all the difference.
Summary and Next Steps
Arthrofibrosis is more than a stiff joint it’s a complex biological and mechanical condition that requires early intervention, active management, and education. Whether you’re a patient or clinician, understanding the science can empower better decisions and better care.
- Identify the type of arthrofibrosis (hot vs cold)
- Use mechanical stretch to support tissue remodelling
- Manage inflammation through icing and nutrition
- Seek supportive physiotherapy input
To learn more, download our free guide or speak to a specialist physio about how the STAK can be integrated into your recovery programme.
You’re not stuck. Progress is possible with the right support and the right tools.