Understanding Arthrofibrosis of the Knee is crucial when post-surgical stiffness and pain persist. This condition causes excessive scar tissue, leading to restricted movement and discomfort beyond the normal healing period.
Though it can feel overwhelming, arthrofibrosis is a recognised medical condition, and with the right approach, recovery is possible. This article will explain what arthrofibrosis is, why it happens, how it’s treated, and what you can do both with professional support and at home to regain your knee function and quality of life.

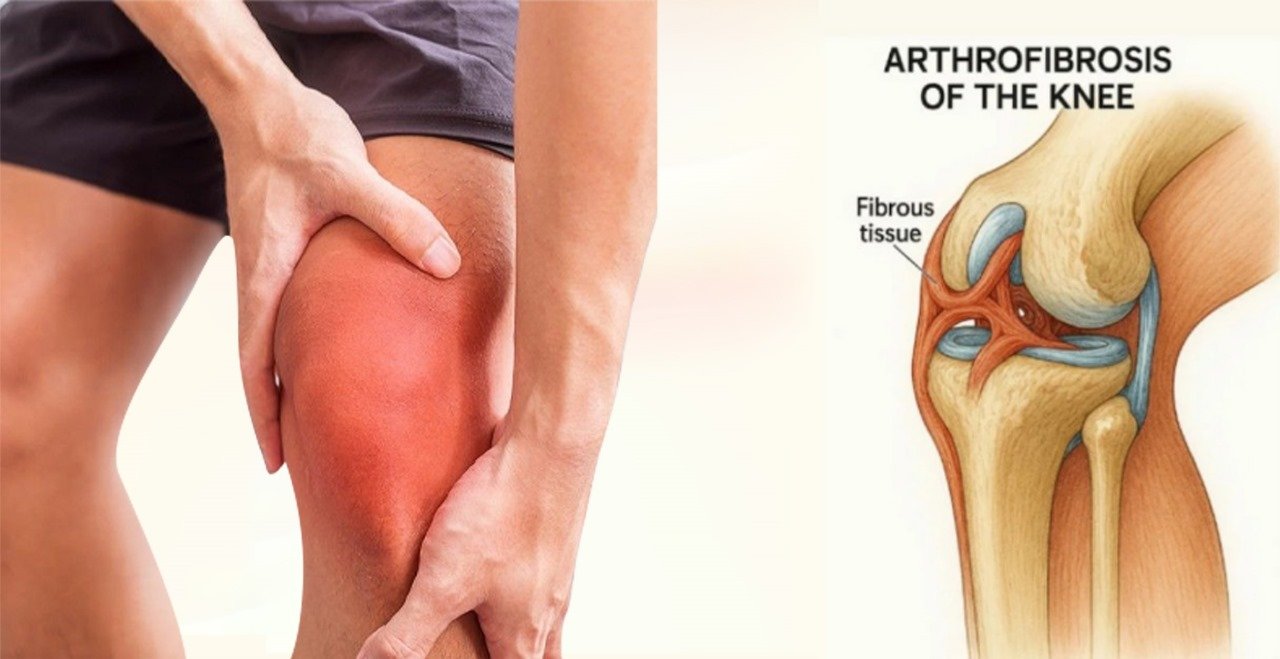
What Is Arthrofibrosis?
Arthrofibrosis is an abnormal healing response in the knee joint. Rather than healing in a flexible, organised way, the body lays down dense, fibrous scar tissue in and around the joint capsule. This scarring restricts movement making the knee feel tight, immobile, or locked in a bent position.
This can happen after:
- Total knee replacement (TKR)
- ACL reconstruction or other ligament surgeries
- Fractures, dislocations, or major trauma
- Repeated injuries or infections
- Severe arthritis
Although scar tissue is a normal part of healing, in arthrofibrosis it becomes excessive and disorganised. The result is a stiff, painful, and swollen knee that doesn’t improve with standard rehabilitation.
📘 Download Your Free Arthrofibrosis Tips Guide
Take your first step today. Download our free resource to help you structure your recovery at home.
⬇ Download NowWhat Are the Symptoms of Arthrofibrosis?
- Limited range of motion (can’t fully straighten or bend the knee)
- Persistent pain or tightness
- Swelling or a feeling of pressure inside the joint
- Loss of function or inability to perform daily activities
- Early plateau in recovery after surgery or injury
One of the key signs is stagnation in progress, even with regular physiotherapy. If your knee seems “stuck” and isn’t responding to treatment after several weeks post-op, it’s worth asking your medical team to investigate further.
What Causes Arthrofibrosis?
Arthrofibrosis can develop for a number of reasons, but it’s ultimately an exaggerated healing response. The body sends an overactive inflammatory and fibrotic signal to the knee, laying down more collagen than necessary. This thickens the soft tissues and restricts the joint.
Contributing factors may include:
- Poor early mobility post-op
- Excessive initial swelling or trauma
- Prolonged immobilisation (e.g. not moving the joint enough)
- Infection or haematoma
- Underlying metabolic or inflammatory conditions
- Individual healing response (some people are simply more prone to fibrosis)
How Is Arthrofibrosis Diagnosed?
Diagnosis is usually based on a combination of:
- Patient history and symptoms
- Physical examination by a physiotherapist or orthopaedic consultant
- Imaging such as MRI or diagnostic ultrasound, though not always necessary
Early detection is key. If arthrofibrosis of the knee is caught in its early stages, it may be reversed with conservative treatment-reducing the need for surgical intervention.

Treatment Options for Arthrofibrosis
1. Physiotherapy
Physiotherapy is the first line of treatment and remains central throughout recovery. The focus is on:
- Stretching the joint capsule to reverse the contracture
- Strengthening surrounding muscles to support the knee
- Manual therapy to reduce swelling, guide movement, and modulate pain
- Home exercise programmes to reinforce mobility between sessions
However, with arthrofibrosis, typical low-intensity rehab may not be enough. Collagen fibres in scar tissue are incredibly resistant to stretch. Research shows that unless sufficient intensity, frequency, and duration are applied, the tissue simply returns to its shortened form (Jacobs & Sciascia, 2011).
Specialist stretching devices, such as the STAK knee stretcher, allow patients to perform prolonged, repeated end-range holds shown to be more effective in remodelling collagen. These tools can be used alongside hands-on physiotherapy to dramatically improve outcomes.
“I often recommend the STAK for patients post-op or post-MUA, especially those with persistent stiffness. It allows them to carry the intensity of physio into their own home, safely and consistently.” – Physiotherapist, NHS Knee Service
2. Manipulation Under Anaesthetic (MUA)
If progress stalls, your orthopaedic consultant may recommend manipulation under anaesthetic (MUA). During this short procedure:
- You are placed under general anaesthetic
- The surgeon gently moves your knee to break down adhesions and scar tissue
- No incisions are made, and you usually return home the same day
MUA is most effective when followed immediately by intensive physiotherapy. Without continued stretching and rehab, the scar tissue may quickly reform.
When is MUA recommended?
- ROM is <90° flexion or >10° extension lag at 6–12 weeks post-TKR
- Progress has plateaued despite compliance with physiotherapy
- Pain and stiffness significantly affect function
Many patients experience a notable improvement in range after MUA – but it’s what happens after that determines long-term success.
3. Arthroscopic or Open Arthrolysis
If both physiotherapy and MUA fail to improve ROM, your consultant may consider surgical arthrolysis, where the scar tissue is cut away using keyhole (arthroscopic) or open surgery. This is typically a last resort and carries greater risks, including infection and further fibrosis.
4. Medical Management
Your team may also look into adjunct treatments:
- Anti-inflammatory medication or short-term steroids
- Nerve desensitisation techniques (for pain control)
- CPM (continuous passive motion) machines, though these are less common today
- Hydrotherapy or warm-pool rehab to aid gentle range of motion

The Role of High-Intensity Stretching and Home-Based Rehab
Perhaps the most overlooked piece of the puzzle is consistent, daily high-quality stretching. Scar tissue is stubborn—it requires time under tension, multiple times a day, often pushing into discomfort (within safe limits).
This is where home-based rehab tools make all the difference. The STAK knee stretcher was developed by orthopaedic physiotherapists specifically for patients recovering from TKR, MUA, and arthrofibrosis. It allows for:
- Safe end-range stretching with measurable intensity
- Flexible use at home between physio sessions
- Control over how far and how long you stretch
- Feedback and structure to help stay motivated
Patients who use tools like STAK often report:
- Better knee bend and straightening
- Reduced pain
- More confidence in managing their rehab
- Faster return to walking, driving, and stairs
While it’s no magic fix, when used correctly and consistently, it can be the difference between progress and plateau.
When to Seek Help
If you’re concerned about your knee recovery:
- You’re more than 6 weeks post-op and still can’t straighten or bend properly
- Pain and stiffness aren’t improving with standard physio
- Your ROM has worsened over time or plateaued early
- You’ve had a MUA and need help maintaining the gains
Speak to your physiotherapist or consultant. Early intervention is crucial. Even if you’re months into recovery, targeted rehab can still make a difference especially when scar tissue hasn’t yet fully matured.
In Summary: There Is Hope
Arthrofibrosis can be frightening, especially when you’re doing everything right and still not improving. But you are not alone and the condition is treatable. With the right support team, the right tools, and the right intensity of rehab, many people go on to regain excellent knee function and quality of life.
The earlier you act, the more options you’ll have so don’t delay in seeking help.
Sara Aspinall, PhD MCSP
Orthopaedic Specialist Physiotherapist
Founder, STAK Orthopaedics Ltd